-
Gcs Powerpoint For Mac카테고리 없음 2020. 2. 7. 20:01
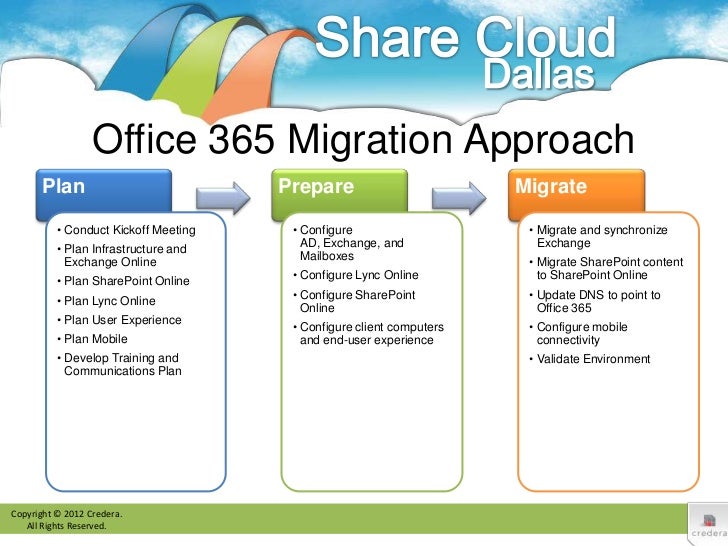
Glasgow Coma Scale. However, at concentrations up to 1 MAC these effects are minimal. Sevoflurane appears to have the best profile. Nitrous oxide is best avoided. Office 365 Famille Premium (Mac) Office 365 Family Premium contains the best of Office software and services. Find Word, Excel, PowerPoint, OneNote, Outlook, Publisher and Access on 5 PC or Mac.
With Medicare cutting an estimated $1.7 Billion in reimbursements in the last two fiscal years combined with the $3,700 manual medical review process putting virtually all part B reimbursement at risk, the need for solid, consistently skilled documentation is at an all time high. The AffordableCare Act brings with it further cuts to reimbursement, tightening the belt further on companies that employ therapists across the nation.
Skilled service providers thatcannot document properly are a liability to their employers and ultimately, themselves. Documentation Bootcamp is a one-day workshop designed to take you through the steps to denial-proof documentation. You will learn how to interpret assessment data for patients on Medicare, set realistic functional goals, and effective interventions to facilitate improvement of function based on accurate assessment data. By strengthening therapy documentation skills, you protectyour patients from prematurely being discharged from deserved care; prevent extra demands upon therapists due to denied claims that have to go through challenging appeals; andensure stable levels of reimbursement for companies that employ therapists. ASHA:Intermediate level, Related Area. Identify the therapist's specific scope of practice as itrelates to patient ID of functional deficits.
Identify key underlying impairment categories that provide the basis for skilled assessment, and ID appropriate tools for assessing them. Utilize assessment of functional deficits and underlyingimpairments to choose an appropriate treatment diagnosis and write a string reason for referral. Select appropriate data from the MDS to formulate SMART goals. Determine appropriate interventions based upon data and assessments. Provide appropriate analysis of update progress notes. Justify current plan of care and future skilled interventionsat mandated intervals.
Evaluate when discharge of care is appropriate, andjustify entirety of care plan from SOC to discharge. Scope of Practice: Identifying Functional and UnderlyingImpairments. PT. OT. SLP.
Justifying Medical Necessity of Skilled Services. Incorporation of medical and treatment diagnosis. Utilizing measurable data from the MDS. Painting a 'bleak picture'- medical necessitystatement.
Hands On Lab. Writing SMART Goals. Specific. Measurable.
Achievable. Realistic. Timely.
Choosing Appropriate Interventions. Based upon findings. Based upon goals. Treatment Intensity (Frequency/Duration). Factors in determining proper intensity.
The dementia factor. When skilled care does not end. Hands On Lab. Update Progress Reports and Recertifications. Further functional assessment.
Maintaining regular underlying impairment measures for further analysis. Justifying progress or lack thereof with proper analysis. Providing appropriate documentation of skilled necessity of care.
Hands On Lab. The Discharge - Why, When, How. Writing a proper discharge summary. Hands On Lab. Since 1991, John Adamson, PT, M.Div., GCS, has worked in physical therapy in a variety of skilled nursing, acute care and home care settings as a clinical specialist, consultant and trainer.
Adamson is involved in ongoing chart audits for state and federal compliance, as well as for reimbursement, and has assisted in Medicare audits, including ADRs and appeals.nullMr. Adamson is a credentialed documentation auditor and recognized as a Master Clinician in documentation and Complex Disease Management, as well as a Geriatric Enhanced Modality Specialist. One of his primary goals is to instruct therapists on the practice of consistent, solid and irrefutable documentation to substantiate medical necessity and prevent denials.
Adamson received his degree in Physical Therapy from Northeastern University in Boston, Massachusetts. DISCLOSURES FINANCIAL: John Adamson is compensated by Summit as an instructor.
NONFINANCIAL: John Adamson has no nonfinancial relationships to disclose. As a national leader in providing high quality live workshops for over a decade, Summit understands that your time and money are extremely valuable - that you don't want to settle for Online Continuing Education that is poor quality, poorly delivered, or won't be accepted by state and national licensing boards. With that as our foundation, we are proud to now offer Online Continuing Education courses that we believe set a new standard of high quality. Leveraging our exceptional teaching faculty that delivers thousands of live workshops each year (with an average customer satisfaction rating of 4.7 out of 5.0), we have now invested in creating the same exceptional Online course experience. We want to make sure that you are 100% comfortable with what you are purchasing, so this is a rundown of the experience you should expect. How do I know if the workshop is approved for CE credit for my profession and state?
We do the work upfront and when you select your profession and state, we only present courses that have CE approval for that profession and state. You can also view the licensing approval by profession on the Product page of any course (middle of page, far right tab of 'CE Credit') If you have further questions regarding your CE approval, please contact Summit Customer Service M-F from 6 a.m. CST at (800) 433-9570 or email ceinfo@summit-education.com. Why aren't all online workshops approved for my profession and state?
The approval of online workshops varies by state and profession, and some licensing boards have longer approval turnarounds than others. How many credits do I receive for an online course? Typically you will receive the same number of credits that you would get at a live workshop. Currently, all of our online workshops range from 1-6 credit hours (with some exceptions based on state and profession).
You can view the licensing approval by profession on the Product page (middle of page, far right tab of 'CE Credit') where you can see the exact number of credit hours for each profession and state. If you have further questions regarding CE credits, please contact Summit Customer Service M-F from 6 a.m. CST at (800) 433-9570 or email customerservice@summit-education.com.
Does Summit report to CE broker? Once you complete your online course, post-course requirements, and the printing of your certificate, please follow the below steps. For ASHA reporting: If you would like to obtain CEUs from ASHA through Summit for completing this course, it is necessary for you to submit a brief ASHA participant form to Summit immediately upon completion of your course. For Live Courses, you will be provided a paper form to return to your Instructor at the end of the workshop. For Online Courses, you will be prompted to fill out an Online form once you have completed the Online Course and post-course test.
For CE Broker reporting: please send an email to ceinfo@summit-education.com with 'report to CE Broker' in the subject line. Send your name, profession, FL license # (AL OT or OH SLP), name of the course, instructor's name, and the date it was completed and Summit will load the credits into CE Broker within 72 business hours. Online Course Content FAQs. Is an outline of the course content available before or during viewing? You can see a course outline on the Product page under the Course Outline tab. After purchase, the course outline is also provided on the media player for watching the course.
How do I access the course manual? Once you have purchased the course, there is a tab at the bottom of the media player where you can download the manual to save or print for your personal use. Manual is located in the 'Resources' tab Are there labs in the course? What do I do if there are labs during the course? Most of our courses have hands-on lab content, varying from minimal to significant. By looking at the Course Outline tab on the Product page, you can see how intensive the labs are for each course. During the lab section, we have invested heavily in providing very strong video content (i.e.
Very tight camera angles) so you can learn along with the live attendees. Depending on the course, you may want to simulate the activities that are presented in the course (which will be noted in the 'Before You Start' section of the media player).
Where can I find who is teaching the course and his/her professional credentials? You can see the instructor and their credentials on the product page under the Instructor Info tab Online Video Experience. How long is the course? Courses range in length from 1-6 hours. You can see the exact length of the course by visiting the course Product page. Will I need any special materials to take the course?
After purchasing, the any special materials or specific advice is listed at the bottom of the 'Course Info' tab. Can I fast-forward or rewind through the online course? For your convenience, you may fast-forward or rewind while watching the course. However, please note you will be required to certify you have watched the entire course to obtain CE credit.
Are there breaks? Can I press pause while watching the course? There are no formal breaks in the video content. However, there is a pause feature to allow taking breaks at your own convenience.
Can I complete the course over several days? How much time do I have to finish the course? Yes, you can always press pause or stop to take a break at your own convenience. Also, if you leave the course, please note where you left so you can pick up where you last finished. However, please remember you need to finish the course and pass your post course test within 30 days (non-subscribers) or before your subscription ends (subscribers). Is the online course interactive? Will I be able to ask questions during the course?
The video that you will be watching is a recorded version of a live workshop. The video captures Instructor answers to participant questions, but there is no opportunity for you to ask questions with the instructor, real time. If you do have questions for the instructor, most instructors have their email address at the end of their presentations. Am I able to re-watch the online courses even after I have completed the post course test and received my certificate?
Once you purchase the online workshop, you have 30 days to view the workshop as many times as you want as well as to review the manual (if you choose not to download while taking the course). For subscribers, your access is unlimited while your subscription is active. Can I get a refund if I don't like the course? We want your experience with Summit to be an enjoyable one. If you purchase an online workshop and don't like it for whatever reason, please stop within the first 30 minutes to receive a full refund. Then call us at (800) 433-9570 to talk with our customer service team to get your refund or a new online course. Test & Certificate.
Will I need to take a post course test? Yes, you are required to successfully pass the post course test to obtain CE credits and certification. This is required by our licensing boards for online courses.
What is the post course test like, what is a passing score, and how many times can I take it? Post course tests are typically 30 True/False and/or multiple choice questions for 6 CE Credits. A passing 'grade' is 75% or higher. You will be able to retake the post course test as many times as necessary to receive a passing grade.
When will I receive my credits and certificate? Once you complete your course evaluation and online test, you will be able to immediately download your certificate. Technical FAQs.
What browsers and Operating system do I need to run for this to work properly? The following are the supported browsers and Operating Systems for the media player to work properly:.
Internet Explorer 10.0+ or Microsoft Edge 20.1+ for Windows 2000, 2003, Vista, XP, Windows 7, Windows 8, Windows 10. Google Chrome 28.0+ for Windows, Mac OSX, or Linux. Mozilla Firefox 23.0+ for Windows, Mac OSX, or Linux. Safari 5.0+ for Mac OSX 10.5 and above Will the media player work on both a Mac and PC? Yes, the online courses will play on both a Mac and PC. The following are the supported browsers and Operating Systems for the media player to work properly:. Internet Explorer 10.0+ or Microsoft Edge 20.1+ for Windows 2000, 2003, Vista, XP, Windows 7, Windows 8, Windows 10.
Google Chrome 28.0+ for Windows, Mac OSX, or Linux. Mozilla Firefox 23.0+ for Windows, Mac OSX, or Linux. Safari 5.0+ for Mac OSX 10.5 and above Can the workshops be played on my phone? You are able to watch the workshops on your phone. Here are the technical requirements to ensure it works properly:. Safari on iPhone. iOS 8+.
iPhone 4s through current. Safari on iPad. iOS 8+. iPad 2 through current.
Chrome on Android. Android 4.0+.
Any running Android 4.0 Are the videos downloadable or streaming? All of the videos stream from the media player. How does the streaming video work?
Live streaming video is content sent in compressed form over the Internet and displayed by the viewer in real time. With streaming video or streaming media, a Web user does not have to wait to download a file to play it. Instead, the media is sent in a continuous stream of data and is played as it arrives. Will I experience any occasional buffering or freezing of the video? Because of our streaming video approach, this rarely happens. If it does, it's typically because of customer internet access quality issues and we will provide troubleshooting tips as well as telephone support from our help desk. Do you provide technical support?
Our help desk is available to assist you by phone Monday through Friday, 6AM to 6PM at (800) 433-9570.
Key points. Traumatic brain injury is common and a major cause of morbidity and mortality worldwide. Management is based on avoidance of secondary injury, maintenance of cerebral perfusion pressure, and optimization of cerebral oxygenation.
Evidence-based guidelines and management protocols help to guide target-driven care and are associated with better outcome. Multimodality monitoring of the injured brain enables individualized therapeutic targets to be set to optimize patient management. Patients with moderate or severe brain injury should be managed in a specialist neurosurgical centre. Epidemiology Traumatic brain injury (TBI) is the leading cause of death and disability in young adults in the developed world. In the UK about 1.4 million patients per year suffer head injuries. Although the majority of injuries are mild, around 10.9% are classified as moderate or severe and many patients are left with significant disability.
Powerpoint For Mac Trial Version
The incidence is increasing in lower income countries, with the World Health Organization predicting that TBI and road traffic accidents will be the third greatest cause of disease and injury worldwide by 2020. In our ageing population the number of elderly patients presenting with TBI has increased and age appears to be an independent risk factor for poor outcome. Consequently TBI presents a major health and socioeconomic problem. TBI is a heterogeneous condition in terms of aetiology, severity, and outcome. The most useful classification of severity is based on the level of consciousness as assessed by the Glasgow Coma Scale (GCS) after resuscitation. The GCS comprises the sum score of the values from three components: eye, motor, and verbal scales (Table ).
TBI is classified as mild (GCS 15–13), moderate (GCS 13–9), and severe (GCS. TBI can be divided into primary and secondary brain injury. The primary injury occurs as a consequence of the initial physical insult. The pattern and extent of damage will depend on the nature, intensity, and duration of the impact. Compression and shearing forces may result in skull fracture, contusions, intracranial haematoma, cerebral oedema, and diffuse brain injury. Microscopically there is cell wall disruption and increased membrane permeability disrupting ionic homeostasis. Axonal tissue is particularly susceptible to injury.
Neurological injury progresses over hours and days, resulting in a secondary injury. Inflammatory and neurotoxic processes result in vasogenic fluid accumulation within the brain, contributing to raised intracranial pressure (ICP), hypoperfusion, and cerebral ischaemia. Much of this secondary injury may be amenable to intervention, as almost one-third of patients who die after a TBI will talk or obey commands before their death.
Secondary injury also occurs as a result of further physiological insults. Hypoxia, hypotension, hyper- or hypocapnia, hyper- or hypoglycaemia have all been shown to increase the risk of secondary brain injury. Acute management This is a crucial period when mortality and morbidity can be influenced by interventions to prevent secondary brain injury. Targeted resuscitation and early specialist management have resulted in a decline in mortality over the last few decades. Pre-hospital care This includes simultaneous assessment, stabilization, and therapeutic interventions.
The priorities are to prevent hypoxia and hypotension, both common findings after trauma. Even a single episode of hypotension is associated with increased morbidity and a doubling of mortality. The number and duration of episodes of hypotension are correlated with mortality. Studies have also found an association between hypoxia and worse outcome. In the USA this has led to pre-hospital guidelines, which include early tracheal intubation for patients unable to maintain their own airway or achieve a target on supplemental oxygen. However, suboptimal intubation and ventilation is associated with worse outcome.
Powerpoint For Mac Torrent
Patients with a moderate or severe TBI should be transferred to a designated trauma centre. Management in the emergency department There is a limited evidence base for much of the management of TBI. A summary of management based on existing consensus guidance and available evidence is shown in Table.
In-hospital resuscitation begins with Advanced Trauma Life Support (ATLS ®) priorities using an ABCDE approach. Assessment of neurological status is based on GCS, pupillary responses, and localizing signs. The mechanism and timing of injuries can provide valuable information and point towards associated injuries.
Major extra-cranial injuries are present in 50% of those with severe TBI. Cervical spine injury is also common with the risk increasing with increasing severity of TBI. Cervical immobilization is required until clearance obtained.
Tracheal intubation remains the gold standard for airway management in patients with a GCS of ≤8. However, the risks, benefits, and timing must be carefully assessed. Pre-existing hypoxia, intracranial hypertension, a potential full stomach, and coexistent injuries including cervical spine instability and maxillofacial injuries may be present. Careful preparation and pre-oxygenation are mandatory.
Airway devices and adjuncts such as laryngeal mask airway, Airtraq ®, or Glidescope ® may be useful, and alternative means of oxygenation and ventilation must be available. Anaesthetic agents should allow rapid control of the airway while attenuating increases in ICP and providing haemodynamic stability.
Propofol and thiopental are commonly used but may cause hypotension. Etomidate has advantages in terms of cardiovascular stability but the possibility of adrenal suppression exists.
Ketamine is popular in trauma patients and recent evidence suggests that its effect on ICP may be limited. For rapid sequence intubation, succinylcholine or rocuronium may be used. Although succinylcholine may produce a small increase in ICP, this is not clinically significant. To obtund the response to laryngoscopy an opiate such as fentanyl is a useful adjunct but there is no evidence to support the use of lidocaine. Adequate sedation and muscle relaxation will reduce cerebral metabolic oxygen requirement (CMRO 2), optimize ventilation, and prevent coughing or straining.
Despite widespread agreement on the principles of early management there is less clarity on resuscitation endpoints, with expert panels offering differing guidelines for management. While the Brain Trauma Foundation (BTF) suggests targeting to avoid hypoxia, the European Brain Injury Consortium (EBIC) targets and the Association of Anaesthetists of Great Britain and Ireland (AAGBI) 13 kPa. Hyper- and hypocapnia are both viewed as potentially avoidable secondary insults. UK guidelines suggest a value of 4.5–5.0 kPa.
Arterial blood pressure (ABP) targets also vary between guidelines. The BTF and EBIC advocate a mean blood pressure (MBP) of 90 mm Hg, while AAGBI targets 80 mm Hg. As the most common cause of hypotension after trauma is haemorrhage, the initial treatment is fluid resuscitation. For most patients an isotonic fluid such as normal saline is suitable. There is some evidence that hypertonic saline may be useful as a resuscitation fluid, with one study showing increased survival in a subgroup of patients with TBI and GCS. GCS 30 min before impact In addition, adult patients who have experienced some loss of consciousness or amnesia since the injury and: Age 65 yr Coagulopathy (history of bleeding, clotting disorder, current treatment with warfarin) Dangerous mechanism of injury (a pedestrian or cyclist struck by a motor vehicle, an occupant ejected from a motor vehicle or a fall from a height of 1 m or five stairs).
GCS 30 min before impact In addition, adult patients who have experienced some loss of consciousness or amnesia since the injury and: Age 65 yr Coagulopathy (history of bleeding, clotting disorder, current treatment with warfarin) Dangerous mechanism of injury (a pedestrian or cyclist struck by a motor vehicle, an occupant ejected from a motor vehicle or a fall from a height of 1 m or five stairs). GCS 30 min before impact In addition, adult patients who have experienced some loss of consciousness or amnesia since the injury and: Age 65 yr Coagulopathy (history of bleeding, clotting disorder, current treatment with warfarin) Dangerous mechanism of injury (a pedestrian or cyclist struck by a motor vehicle, an occupant ejected from a motor vehicle or a fall from a height of 1 m or five stairs). GCS 30 min before impact In addition, adult patients who have experienced some loss of consciousness or amnesia since the injury and: Age 65 yr Coagulopathy (history of bleeding, clotting disorder, current treatment with warfarin) Dangerous mechanism of injury (a pedestrian or cyclist struck by a motor vehicle, an occupant ejected from a motor vehicle or a fall from a height of 1 m or five stairs).
Imaging The investigation of choice is CT scanning. Early imaging reduces time to detection of life-threatening complications and is associated with better outcomes. The incidence of radiological abnormalities increases with the severity of injury, and various criteria, such as those recommended by the National Institute of Clinical Excellence (Table ), have been developed to determine who requires CT scan.
CT imaging of the cervical spine should be performed at the same time. MRI studies are rarely used in the acutely ill, as they are logistically more complex and take longer. MRI is useful if a penetrating injury with a wooden object is suspected.
Advanced MRI (diffusion tensor imaging) allows visualization of white matter tracts and quantification of axonal damage. Skull X-rays are useful only as part of a skeletal survey in children with non-accidental injury. Additional imaging may be necessary to identify occult life-threatening injuries. As brain injury evolves over time, repeat imaging is commonly indicated and always necessary if there is clinical deterioration or an increase in ICP. Transfer National guidelines on the transfer of patients with TBI are available. Initial resuscitation and stabilization of the patient should be completed before transfer.
Although neurosurgical transfers are time-critical, the risks of delayed transfer must be balanced against that of an unstable patient or ill-prepared transfer team. An experienced and appropriately trained doctor with dedicated and skilled assistance should accompany patients with TBI.
There must be means of communication with the neurosurgical centre and base hospital, a suitable transfer vehicle, full monitoring, including invasive arterial pressure, capnography and urinary catheter, resuscitation equipment, necessary drugs, and back up supplies in case of ventilator or pump failure. Management priorities remain maintenance of oxygenation and ABP and minimizing increases in ICP. Patients who are persistently hypotensive despite resuscitation should not be transferred until the cause established and the patient stabilized. Patients with a GCS of ≤8 should be intubated and ventilated, aiming for and a value of 4.5–5.0 kPa with adequate sedation, analgesia, and muscle relaxation.
AAGBI indications for intubation and ventilation and a transfer checklist are shown in Tables. Respiration and Airway clear? Airway protected adequately? Intubation and ventilation required? Circulation MBP 80 mm Hg, pulse. Respiration and Airway clear? Airway protected adequately?
Intubation and ventilation required? Circulation MBP 80 mm Hg, pulse. Respiration and Airway clear?
Airway protected adequately? Intubation and ventilation required? Circulation MBP 80 mm Hg, pulse.
Respiration and Airway clear? Airway protected adequately?
Intubation and ventilation required? Circulation MBP 80 mm Hg, pulse. Good communication between the referring clinician, transfer team, and the neurosurgical centre is paramount. Anaesthesia for trauma craniotomy About one-third of patients with severe TBI need neurosurgical intervention. Rapid treatment is crucial.
Acute subdural haematomas in patients with a severe TBI have 90% mortality if surgical evacuation occurs 4 h after injury compared with 30% for those evacuated earlier. Perioperative management should be a seamless continuation of the resuscitation process already begun and an opportunity to correct pre-existing secondary insults. Surgery and anaesthesia predispose the patient to additional risks such as hypotension because of blood loss or the effect of anaesthetic agents. Essential monitoring includes ECG, capnography, temperature, and urine output.
Invasive arterial pressure allows beat-to-beat monitoring of ABP and regular assessment of arterial blood gases and glucose. Central venous access may be useful for resuscitation and administration of vasoactive drugs. ICP monitoring is recommended for patients with TBI who require non-neurosurgical intervention. The goals of anaesthesia are Anaesthesia and analgesia are essential, as surgical stimuli can increase cerebral blood flow (CBF), CMRO 2, and ICP. Despite important differences between the effects of i.v. And volatile anaesthetic agents on cerebral physiology there is little evidence to support the use of one over the other.
All volatile agents reduce CMRO 2 and may produce cerebral vasodilation, resulting in increased CBF and ICP. They also impair CO 2 reactivity. However, at concentrations up to 1 MAC these effects are minimal. Sevoflurane appears to have the best profile. Nitrous oxide is best avoided. Agents reduce CMRO 2, CBF, and ICP.
However, propofol can cause significant hypotension and reduce CPP. Neuromuscular drugs are recommended to prevent coughing or straining.
optimization of cerebral perfusion pressure (CPP) and the prevention of intracranial hypertension;. adequate anaesthesia and analgesia;. prevention of secondary insults by adequate oxygenation, normocapnia, and avoidance of hyper- or hypoglycaemia and hyperthermia. Patient positioning is usually dictated by surgical access. However, flexion or rotation of the head and the Trendelenberg position may increase ICP in patients with impaired intracranial compliance.
Overly tight tracheal tube ties or cervical collars can also obstruct venous drainage. Ventilation should be controlled to maintain oxygenation and normocapnia as confirmed by ABG analysis.
Intraoperative hypotension is associated with a three-fold increase in mortality. As discussed previously, i.v. Fluids are the primary means to control ABP but debate continues as to the type and volume of choice. There may be a temporary, sometimes severe, decrease in BP after surgical decompression, and administration of vasopressor agents may be necessary to maintain BP and CPP during periods of instability. Several studies have shown an association between hyperglycaemia and poor neurological outcome in patients with TBI. The optimal target glycaemic range is yet to be defined but, currently, the literature supports targeting intermediate glucose levels in the range of 6–10.0 mmol l −1.
Patients should have frequent glucose monitoring and hypoglycaemia must be prevented. Management of ICP Intracranial hypertension reduces cerebral perfusion and results in cerebral ischaemia. Consensus guidelines recommend treatment of an ICP 20–25 mm Hg. Measurement of ICP allows early detection of evolving mass lesions and enables the calculation of CPP from the relationship CPP = MAP − ICP.
The primary goal of an adequate CPP is to maintain CBF and tissue oxygenation and its manipulation has become central to the management of TBI. BTF guidelines initially adopted a CPP of 70 mm Hg but this was subsequently reduced when studies confirmed a greater risk of pulmonary complications with aggressive fluid and vasopressor therapy. Current consensus is a target of 60 mm Hg.
ICP can be controlled by a variety of methods. Hyperventilation A reduction in causes cerebral vasoconstriction, reducing CBV and ICP. Although once widely used, hyperventilation has been shown to exacerbate cerebral hypoperfusion and may result in ischaemia. Moderate hyperventilation to a value of 4.0–4.5 kPa is reserved for those with intractable intracranial hypertension and should be guided by monitoring such as jugular venous oxygen saturation to ensure adequate cerebral oxygenation.
Hyperosmolar therapy This is particularly useful for acute increases in ICP. Mannitol remains the most commonly used agent. The effective dose is 0.25–1 g kg −1, usually given as a 20% solution. Intermittent boluses appear to be more effective than continuous infusions. However, care must be taken to prevent serum osmolarity increasing above 320 mOsm l −1, as this has been associated with neurological and renal complications. Other potential complications include hypotension, intravascular volume depletion, hyperkalaemia, and rebound intracranial hypertension. The use of hypertonic saline is increasing.
It has fewer side-effects and may control ICP refractory to mannitol. Hypertonic saline acts predominantly through the osmotic shift of fluid from the intracellular to the intravascular and interstitial space. It may also improve CBF and myocardial performance and may have immune-modulatory effects.
Various concentrations are available from 1.7 to 29.2% and numerous regimens described, although a dose of 2 ml kg −1 of a 5% solution is typical. This can be repeated, providing the plasma osmolarity remains. St George's neurocritical care unit management algorithm for patients with severe traumatic brain injury. ICP, intracranial pressure; CPP, cerebral perfusion pressure. The purpose of continuing care is to provide optimum opportunity for brain recovery. Maintenance of oxygenation, normocapnia, and haemodynamic stability is essential.
Adequate sedation and analgesia reduces pain, anxiety, and agitation and facilitates mechanical ventilation. Multimodality monitoring of the injured brain is useful to tailor individual patient care.
Advanced monitoring may include cerebral oxygenation, measurement of CBF, microdialysis, and electrophysiological monitoring. Early nutritional support is associated with better outcomes and enteral administration is preferable.
Appropriate metabolic monitoring is essential, as hyperglycaemia is associated with secondary ischaemic injury. Blood glucose should be monitored, but optimal targets for glycaemic control are yet to be defined. However, as with perioperative management, intermediate glucose levels in the range of 6–10.0 mmol l −1 are usually targeted. Hypoglycaemia must be avoided. Seizure activity is relatively common, occurring both early and late after TBI.
Seizures increase CMRO 2 and are associated with increased ICP. Although there is little evidence for prophylactic anticonvulsants, some advocate their use in high-risk groups such as those with depressed skull fractures. Patients with TBI are at significant risk of thrombo-embolic events. Options for prevention include mechanical (graduated compression stockings or intermittent pneumatic compression), pharmacological (low-dose or low-molecular-weight heparin) prophylaxis, or a combination of both. Most would avoid pharmacological thromboprophylaxis for 24 h after neurosurgical intervention. Additional care includes peptic ulcer prophylaxis, physiotherapy, and full hygiene care. Summary TBI is common and a major public health problem.
Despite a progressive and significant reduction in mortality no single treatment has been shown to improve outcome. Management continues to be focused on prevention of secondary injuries and maintenance of CPP.
National guidelines and management algorithms seem to be associated with better survival but ignore individual patient variability and injury-specific factors. Declaration of interest None declared.